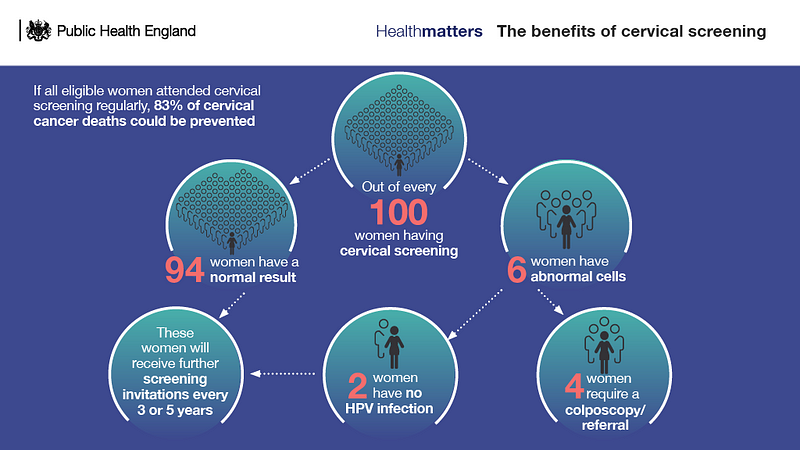
Figures published by NHS Digital show that by 31 March 2017, the percentage of eligible women (aged 25 to 64) who were recorded as screened adequately was 72.0%. This compares with the 72.7% at 31 March 2016 and 75.4% at 31 March 2012 who were screened.
Given this decline in uptake, Public Health England has decided to launch a national cervical screening campaign in March of 2019. This is to raise more awareness around the subject of cervical cancer and known causes such as the Human Papilloma Virus (HPV) and related diseases to get more women participating.
Important changes
Cervical screening is evolving and there have been some very important changes made. Some of these important changes include:
The introduction of the HPV primary screening test.
HPV primary screening will be implemented into the NHS Cervical Screening Programme, with full coverage to be achieved across the whole of England by 2020.
The possibility of using a home-based self-sample, which is being considered in a UK National Screening Committee consultation.
The issue affecting much of the effectiveness of organized screening for cervical cancer is the lack of participation by certain demographics of women. This is proven by the fact that the majority of cervical cancers arise in women who are either never-screened or under‐screened.
The good news with the addition of HPV testing is that it is likely to replace colposcopies/pap tests in many developed countries.
Although it is true that HPV testing through self‐collected samples is slightly less sensitive and less specific than HPV testing by a qualified medical practitioner, it has the potential to overcome some of the barriers involved with conventional screening and encourages the participation from demographics who have previously never screened.

Changes in HPV vaccination to include males.
The female programme has already been a success in reducing the prevalence of HPV strains 16 and 18, the main cancer-causing types, by over 80%.
There are now also plans to broaden the scope of this programme to include the vaccination of adolescent males.
The vaccine will not only help to protect the male patients from HPV-related diseases – such as oral, throat and anal cancer; but by having more of the population vaccinated -known as ‘herd immunity’- this will also help reduce the overall number of cervical cancers in women.
This progress means that we will be able to reduce cervical and other related cancers in both men and women in the future.
Pilots to trial text messaging reminders.
This is a progressive move for the NHS, though even greater integration with communications technology for screening reminders would be welcome.
There are many possibilities for scheduling automated reminders, it simply requires the decision-makers to allow this progression. This would open the way for a more efficient and cost-effective process, leading to more patient engagement with the available services.
By Medicalchain’s Tim Robinson

